- Arbitration
- Banking & Finance
- Capital Markets
- Commercial
- Competition
- Construction & Infrastructure
- Corporate / Mergers & Acquisitions
- Corporate Services
- Corporate Structuring
- Digital & Data
- Dispute Resolution
- Employment & Incentives
- Family Business & Private Wealth
- Innovation, Patents & Industrial Property (3IP)
- Insurance
Find a Lawyer
Book an appointment with us, or search the directory to find the right lawyer for you directly through the app.
Find out more
Real Estate & Construction and Hotels & Leisure
Real estate, construction, and hospitality are at the forefront of transformation across the Middle East – reshaping cities, driving investment, and demanding increasingly sophisticated legal frameworks.
In the June edition of Law Update, we take a closer look at the legal shifts influencing the sector – from Dubai’s new Real Estate Investment Funds Law and major reforms in Qatar, to Bahrain’s push toward digitalisation in property and timeshare regulation. We also explore practical issues around strata, zoning, joint ventures, and hotel management agreements that are critical to navigating today’s market.
As the landscape becomes more complex, understanding the legal dynamics behind these developments is key to making informed, strategic decisions.
2025 is set to be a game-changer for the MENA region, with legal and regulatory shifts from 2024 continuing to reshape its economic landscape. Saudi Arabia, the UAE, Egypt, Iraq, Qatar, and Bahrain are all implementing groundbreaking reforms in sustainable financing, investment laws, labor regulations, and dispute resolution. As the region positions itself for deeper global integration, businesses must adapt to a rapidly evolving legal environment.
Our Eyes on 2025 publication provides essential insights and practical guidance on the key legal updates shaping the year ahead—equipping you with the knowledge to stay ahead in this dynamic market.
The leading law firm in the Middle East & North Africa region.
A complete spectrum of legal services across jurisdictions in the Middle East & North Africa.
-
Practices
- All Practices
- Banking & Finance
- Capital Markets
- Commercial
- Competition
- Construction & Infrastructure
- Corporate / Mergers & Acquisitions
- Corporate Services
- Corporate Structuring
-
Sectors
-
Country Groups
-
Client Solutions
Today's news and tomorrow's trends from around the region.
17 offices across the Middle East & North Africa.
Our Services
 Back
Back
-
Practices
- All Practices
- Banking & Finance
- Capital Markets
- Commercial
- Competition
- Construction & Infrastructure
- Corporate / Mergers & Acquisitions
- Corporate Services
- Corporate Structuring
- Digital & Data
- Dispute Resolution
- Employment & Incentives
- Family Business & Private Wealth
- Innovation, Patents & Industrial Property (3IP)
- Insurance
- Intellectual Property
- Legislative Drafting
- Private Client Services
- Private Equity
- Private Notary
- Projects
- Real Estate
- Regulatory
- Tax
- Turnaround, Restructuring & Insolvency
- Compliance, Investigations and White-Collar Crime
-
Sectors
-
Country Groups
-
Client Solutions
- Law Firm
- /
- Insights
- /
- Law Update
- /
- November 2018
- /
- Universal Healthcare Coverage in Bahrain
Universal Healthcare Coverage in Bahrain
Noor Al Rayes - Partner, Head of Litigation - Bahrain - Dispute Resolution
Hussain Osman
After a long back and forth between the legislative and executive branches of Government, Law No (23) of 2018 Issuing the Health Insurance Law (‘HIL’) finally saw the light of day after receiving royal assent on 30 May 2018.
In line with Goal three of the United Nation’s Sustainable Development Goals, ‘Good health and well-being for people to ensure healthy lives and promote well-being for all at all ages’;, the Kingdom of Bahrain (‘KOB’) has introduced a universal health coverage scheme giving patients the freedom of selecting their caregiver of choice. This pragmatic approach to healthcare will be funded by an health insurance fund cumulating its capital from diverted citizen allocations and annual subscriptions paid by or on behalf of foreigners and their subjects. Military personnel and diplomats are to be alternatively covered in lieu of the national scheme by their respective employers.
The fund
Article 4 of HIL dictates the establishment of the Health Insurance Fund (‘Fund’) governed by the Chairman, Ministers of Health, Finance, Labour and five elected members chosen by the Supreme Council for Health (‘SCH’) These board members are vested with the prime mandate of bankrolling health benefits for subscribers to the proposed health insurance scheme. The Fund, as an entity, has been tasked with the following:
- enter into contracts with health service providers to provide health benefits to the beneficiaries for whom the Fund provides insurance coverage;
- collect and analyse the data, information and statistics on persons for whom the Fund provides insurance coverage;
- set the rules and procedures for collecting the health insurance contributions due to the Fund in coordination with other concerned government agencies;
- possess movable and immovable assets, and manage and invest any of the Fund’s resources;
- coordinate with the SCH and concerned authorities with respect to all matters related to the application of the health insurance system;
- propose programmes and policies that will enhance the health insurance system with regard to the matters outside the competence of the Fund, and providing them to the stakeholders;
- organise training and educational courses and programmes aimed at raising awareness of the provisions hereof, spreading a culture about all aspects of the health insurance system, conducting research and studies in this field, and benefitting from its outcomes in coordination with the SCH;
- opine on the draft laws related to the health insurance system and the regulations and decisions issued by other relevant bodies in coordination with the SCH;
- study the relevant applicable laws and regulations in order to find out whether or not they include any provisions that hinder the advancement of the health insurance system, and propose amendments thereto in accordance with the constitutional mechanisms in place; and
- receive and examine complaints and reports related to the insurance coverage provided by the Fund, determine their seriousness, and take the necessary measures.
The Fund shall primarily rely on appropriations allocated by the government and its return on investment in order to finance the abovementioned mandates. A percentage of licensing fees collected by the National Health Regulatory Authority (“NHRA”) for the establishment or renewal of private health institutions will also be transferred to the Fund. Donations, subsidies and any other resources may be accepted subject to the Fund’s board of directors determining their concordance with the Fund’s objectives.
A key resolution will be issued by the SCH in coordination with the Central Bank of Bahrain laying down the provisions, rules and conditions of health insurance coverage and its valid term. Insurance providers would then be expected to register on a newly established Insurance Service Provider Register at the NHRA. Listed insurance coverage providers will be authorised to issue health insurance cards for each beneficiary. Health service providers licensed by the NHRA may participate in the provision of the services covered under the mandatory health registered insurance system by entering into contracts with registered insurance coverage providers to provide all or some of the health benefits to the beneficiaries.

The health insurance system: health data and informatics
With the instatement of the new regime, a series of elements will be put in place by the SCH to enable the steady functioning of this new method of providing healthcare. Under the auspices of the SCH, a tripartite alliance of data banks will prove key for administering the delivery of healthcare.
Health Information and Knowledge Management Center
The Health Information and Knowledge Management Centre (‘Centre’) shall undertake the duties of collecting, analysing and processing health related data and authorising those permitted to process or receive health related data. The Centre will set up an online portal that interconnects insurance coverage providers and health service providers. The centralisation of data in one portal will aid the Centre in gathering information and statistics related to beneficiaries, providers of coverage and health service providers and their transactions, in order monitor and verify compliance with the provisions of HIL.
Unified Electronic Medical Record
Each beneficiary shall have an electronic medical record containing all his or her data, particularly health related data as well as data that may be used as a basis for claiming financial benefits. A decision shall be issued by the SCH identifying such data, rules and guarantees to be contained in the record in order to ensure the protection and confidentiality of the recorded data.
The Centre shall link healthcare providers to the electronic medical record after being granted access by the SCH.
National Health Data Dictionary
Comprising of a detailed nomenclature system of health related terms, medical coding and their definitions, these clinically coded terms are classified into categories and arranged in a special order to be a reference for healthcare institutions and insurers by using a standardised language that allows technical systems to receive, send, store, display, retrieve or process the dictionary contents.
Mandatory health insurance
Section (2) of the HIL states that mandatory health insurance shall apply to all national citizens, residents and visitors. Non Bahraini women who married Bahraini men, sons of Bahraini women married to non Bahraini women fall within the category of national citizens who are entitled to mandatory health insurance.
An employer shall cover his non Bahraini employees with the mandatory health insurance, in addition to their dependents of their family members, in case the employment contract provides for this, through the conclusion of a health insurance contract with any of the insurance coverage provider.
The Fund will cover mandatory health insurance subscriptions for national citizens and the equivalent as well as for non Bahrainis who hold positions in any government body. Residents and expatriates with valid subscriptions under the mandatory health package will have access to insurance coverage under the mandatory health insurance.
Unemployed residents, authorised workers without employers (i.e. flexi permit holders), sponsors and visitors are expected to pay the subscription in order to receive health coverage for themselves and dependents.
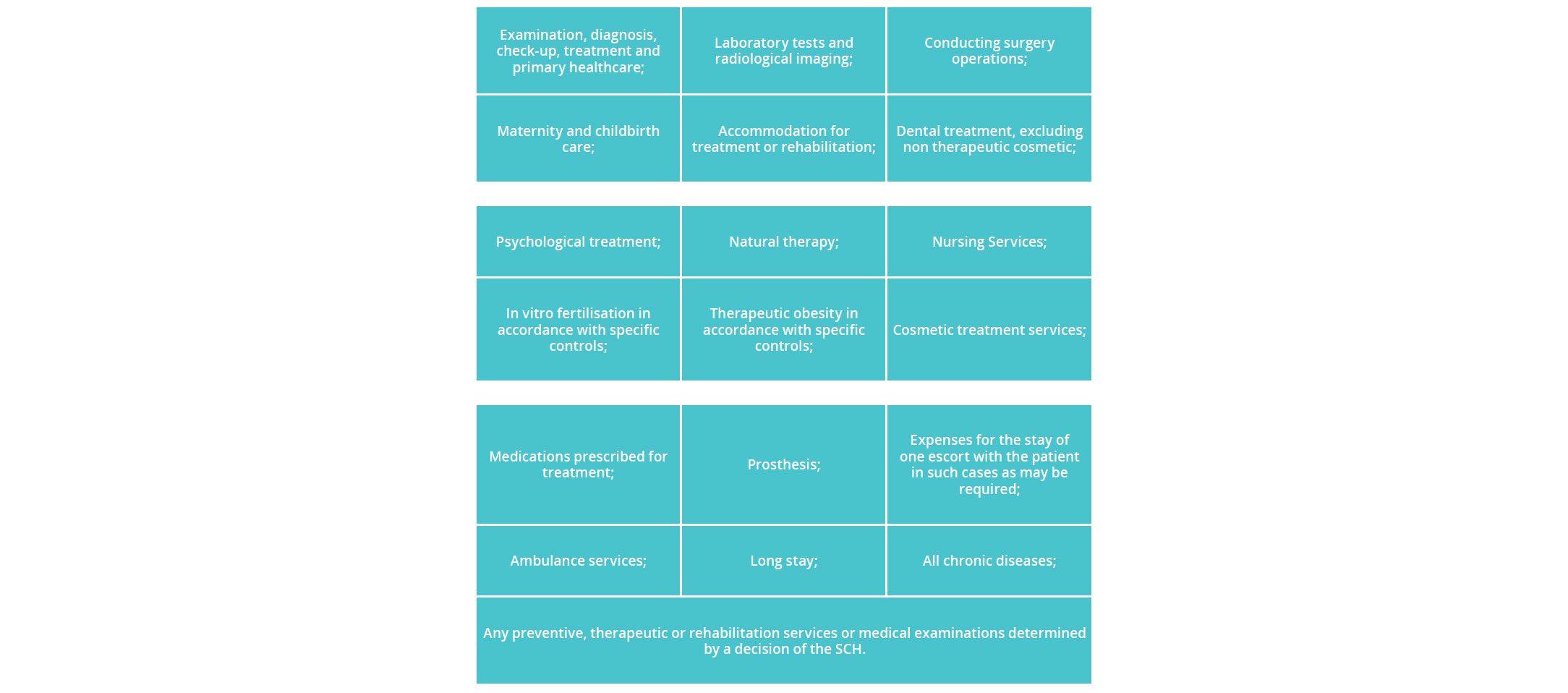
Article (37) of the HIL lists the following preventive, therapeutic and rehabilitative services and medical examinations assured by the coverage items.
Mandatory coverage will also cover prescribed medication. A voluntary insurance package may also be purchased at a subsidised rate for national citizens and residents from an authorised health insurance provider.
Where does this leave government health care providers?
The HIL has stipulated governance by trusteeship for government health institutions. The board of trustees will be tasked with managing the affairs of government health institutions, in line with the KOB’s national health policy and the health insurance financing system. This newfound independence will place government hospitals in the private sphere of competition, placing higher demand on quality and administration of care.
Violations and penalties
Regulatory Violations
If and when a violation is proven, the NHRA shall order the offender to cease and eradicate the effects of the offence immediately or within a set period of time. Subject to non compliance, an adequate justification shall fine the violator with one of the following actions set out under Article (76):
- imposition of a fine calculated on a daily basis to enforce the offender to cease the violation and to eradicate its causes or effects. The fine shall not exceed 300 Dinars per day when committing the violation for the first time, and 1,000 Dinars when committing more violations within three years from the date of the decision on the previous violation. In all cases, the sum of all fines shall not exceed 20,000 Dinars; or
- impose a total fine not exceeding 20,000 Dinars; or The fine shall be determined in view of the severity of violation, negligence of the offender to eradicate it, the benefits gained, and the damage incurred by third parties as a result.
- if the NHRA deems that the investigation revealed a criminal offence, the documents shall be referred to the Public Prosecution.
The Central Bank of Bahrain and the Labour Market Regulatory Authority shall take over the competencies and authority of inspection, investigation and accountability in relation to any regulatory violations committed by the insurance coverage providers or an employer in contravention to their obligations.
“The Fund will cover mandatory health insurance subscriptions for national citizens and the equivalent and for non Bahrainis who hold positions in any government body.”
Criminal Responsibility
The law has stipulated for very person who i) deliberately submits false, misleading or contrary information on records or documents at his disposal to; or ii) withholds any data, information, records or documents that he shall furnish or allow access thereto to perform the function of the SCH or to the Centre; or iii) hinders the NHRA’s inspectors from performing their work, or obstructs any investigation performed by the NHRA, a fine not less than 500 Dinars and not more than 50,000 Dinars. In cases other than recidivism, the offences set above may be compounded by paying the minimum fine provided in accordance with the controls and procedures to be set by the SCH.

Stay updated
To learn more about our services and get the latest legal insights from across the Middle East and North Africa region, click on the link below.